Hyponatremia Risk Assessment Calculator
Hyponatremia occurs when serum sodium levels fall below 135 mmol/L. This calculator helps assess your risk level based on sodium concentration and associated symptoms.
Risk Assessment Results
Quick Takeaways
- Hyponatremia lowers serum sodium below 135mmol/L and can be acute (<48h) or chronic.
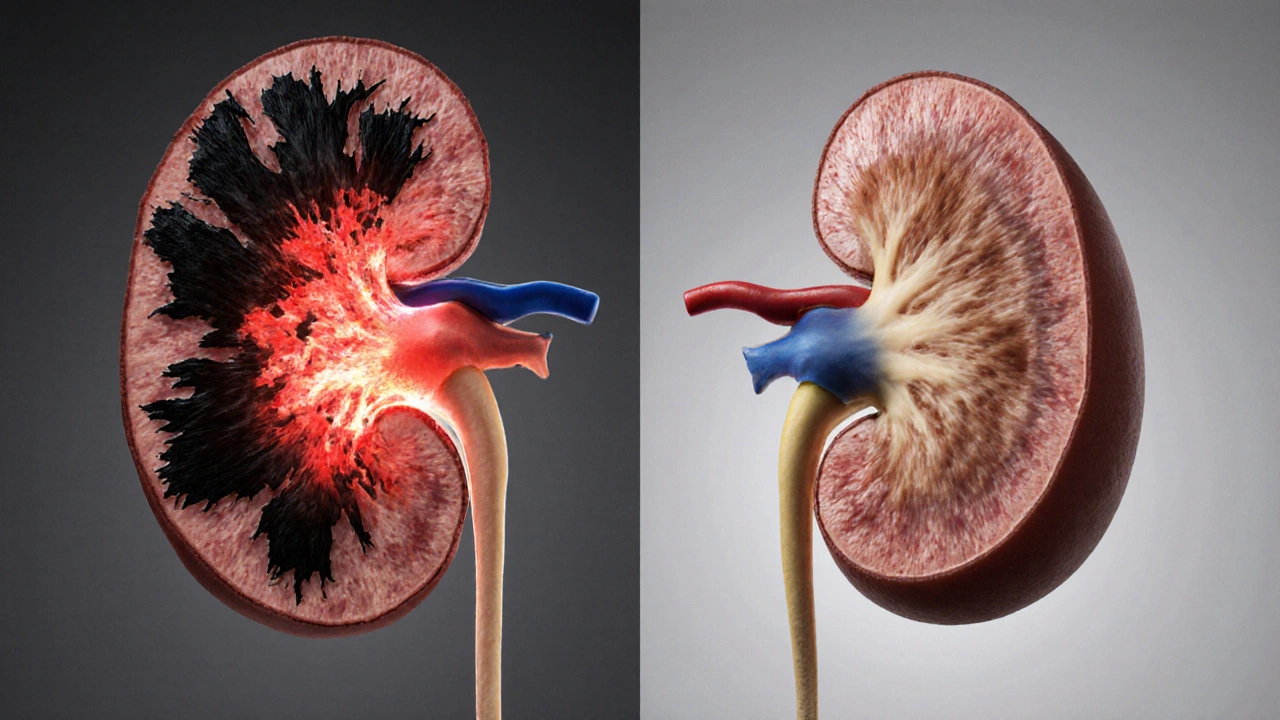
- Both acute and chronic low‑sodium states strain the kidneys, reducing glomerular filtration rate (GFR) and promoting tubular injury.
- Patients with chronic kidney disease (CKD) are especially vulnerable; hyponatremia accelerates progression toward end‑stage renal disease.
- In transplantation, uncontrolled hyponatremia raises peri‑operative complications and can disqualify donors or recipients.
- Early identification, tailored fluid‑management, and careful correction protocols improve outcomes for transplant candidates.
What Is Hyponatremia?
Hyponatremia is an electrolyte disorder where serum sodium concentration falls below the normal reference range of 135‑145mmol/L. It results from an excess of water relative to sodium, not from a shortage of sodium itself. Common triggers include excessive hypotonic fluid intake, syndrome of inappropriate antidiuretic hormone secretion (SIADH), heart failure, liver cirrhosis, and certain diuretics. The condition is classified by onset (acute vs chronic) and by volume status (hypovolemic, euvolemic, hypervolemic).
How Sodium Balance Impacts Kidney Function
The kidneys regulate extracellular fluid osmolality by filtering plasma, reabsorbing sodium, and excreting free water. When sodium levels dip, the renal tubules respond by increasing water reabsorption via antidiuretic hormone (ADH) signaling. Persistent ADH activation constricts the medullary gradient, leading to reduced water clearance and a cycle of further dilution.
Prolonged low‑sodium environments cause tubular cell swelling, disrupt ATP production, and stimulate inflammatory cytokines. Over time, these changes lower the Glomerular Filtration Rate (GFR), the core metric of kidney performance. Even modest drops in GFR (e.g., from 90 to 70mL/min/1.73m²) signal early renal stress and predict faster CKD progression.
Acute vs Chronic Hyponatremia: Renal Implications
Acute hyponatremia (<48h) often follows rapid water overload, such as marathon drinking or postoperative fluid therapy. The kidneys may initially compensate, but the sudden osmotic shift can cause cortical tubular necrosis and a sharp rise in serum creatinine.
Chronic hyponatremia (>48h) allows adaptive cellular mechanisms, yet the kidneys remain under constant osmotic load. Long‑term adaptation includes reduced urea recycling, altered expression of sodium‑potassium pumps, and a subtle rise in albuminuria.
| Feature | Acute (<48h) | Chronic (>48h) |
|---|---|---|
| Serum Sodium Drop | Rapid (≥10mmol/L) | Gradual (≤10mmol/L) |
| GFR Change | Sudden ↓ (10‑20%) | Progressive ↓ (5‑10% per year) |
| Tubular Injury Markers | Elevated NGAL, KIM‑1 | Low‑grade rise in N‑acetyl‑β‑D‑glucosaminidase |
| Clinical Symptoms | Headache, nausea, seizures | Fatigue, mild confusion, gait instability |
Hyponatremia and Chronic Kidney Disease
Patients with CKD experience impaired sodium handling due to loss of nephrons and altered tubular responsiveness. Studies from 2023‑2024 show that CKD patients with serum sodium <130mmol/L have a 1.8‑fold higher risk of reaching end‑stage renal disease within three years compared with those maintaining normal sodium levels.
Low sodium also worsens volume overload, a common CKD problem, by stimulating ADH release. The resulting hyponatremic state intensifies interstitial edema, aggravates hypertension, and fuels proteinuria-each a recognized accelerator of renal decline.
Impact on Kidney Transplantation
Transplant programs screen both donors and recipients for electrolyte stability. Hyponatremia in a donor can signal underlying liver disease or heart failure, both of which increase the likelihood of delayed graft function (DGF) after implantation.
For recipients, pre‑operative hyponatremia is linked to higher rates of peri‑operative hypotension, prolonged ventilation, and acute rejection episodes. A multicenter analysis in 2024 reported that recipients corrected to ≥135mmol/L before surgery had a 22% reduction in DGF compared with those left untreated.
Immunosuppressive regimens (e.g., tacrolimus) can cause tubular toxicity, and when combined with hyponatremia, the risk of nephrotoxicity spikes. Therefore, maintaining optimal sodium levels is a non‑negotiable step in the transplant work‑up.

Managing Hyponatremia in Transplant Candidates
Effective management hinges on three pillars: diagnosing the underlying cause, controlling free‑water excess, and correcting sodium at a safe rate.
- Identify the etiology: Measure serum and urine osmolality, assess volume status, and test ADH levels. Distinguish SIADH (euvolemic, high urine osmolality) from hypovolemic causes (low urine sodium).
- Fluid restriction: For SIADH, limit intake to 800‑1000mL/day. In hypovolemic states, replace with isotonic saline to restore volume before addressing sodium.
- Pharmacologic options: Vaptans (e.g., tolvaptan) antagonize vasopressin receptors and promote free water excretion, useful when fluid restriction fails. Demeclocycline can also blunt ADH action but has renal toxicity concerns, so reserve for refractory cases.
- Correction rate: Aim for ≤8mmol/L increase in the first 24h to avoid osmotic demyelination. Use serial sodium checks every 4-6h during the initial phase.
Post‑correction, maintain sodium with balanced diet (400-600mmol/day of sodium) and adjust diuretic dosing based on GFR trends.
Monitoring and Follow‑up Strategies
After correction, close monitoring ensures the kidneys stay stable. Recommended protocol:
- Daily serum sodium and creatinine for the first week.
- Weekly GFR estimation (eGFR) for the first month.
- Urine sodium and osmolality every two weeks until stabilisation.
- Re‑evaluate volume status at each clinic visit; aim for euvolemia without over‑diuresis.
For transplant recipients, integrate sodium checks into the immunosuppression monitoring schedule. Any upward trend in serum creatinine >0.3mg/dL warrants a renal ultrasound to rule out obstruction, which can be aggravated by fluid shifts.
Frequently Asked Questions
Can mild hyponatremia (<130mmol/L) be ignored in kidney transplant candidates?
No. Even mild hyponatremia signals impaired water handling and can increase peri‑operative complications. Correcting to normal levels before surgery improves graft function and reduces hospital stay.
What is the safest correction speed for chronic hyponatremia?
Aim for a rise of no more than 8mmol/L in the first 24hours and less than 18mmol/L over 48hours. This minimizes the risk of osmotic demyelination syndrome.
Do vaptans interfere with immunosuppressive drugs?
Tolvaptan is metabolised by CYP3A4, the same pathway as tacrolimus. Dose‑adjustment of tacrolimus may be needed, and therapeutic drug monitoring should be intensified.
How often should serum sodium be checked after a transplant?
Daily for the first week, then every 3‑5days during the first month, and weekly thereafter until the patient stabilises.
Is there a link between hyponatremia and long‑term graft survival?
Yes. Cohort studies from 2022‑2024 show that patients with persistent post‑transplant hyponatremia have a 15‑20% higher risk of graft loss at five years, likely due to chronic tubulointerstitial injury.



Rebecca Mikell
October 8, 2025 AT 18:46Hyponatremia is something many patients don’t realize can sneak up on them until it’s already affecting their kidneys.
When serum sodium drops below 135 mmol/L the body’s ability to concentrate urine gets compromised.
This can lead to fluid overload, which is a major red flag for anyone waiting on a transplant.
The kidneys rely on a delicate sodium gradient to filter waste efficiently, so low sodium messes with that balance.
In transplant candidates, even mild hyponatremia can raise the risk of delayed graft function after surgery.
That’s why pre‑operative labs should always flag a sodium level under 135 and trigger a deeper work‑up.
Treating the underlying cause – whether it’s a medication, SIADH, or excess water intake – should be the first step.
Fluid restriction, if done under supervision, can gently raise sodium without causing abrupt shifts that might harm the brain.
Some centers even use hypertonic saline in a controlled setting to correct severe cases before the operation.
It’s crucial to avoid rapid correction, because osmotic demyelination syndrome is a scary complication that can undo any transplant gains.
Monitoring urine output and adjusting immunosuppressive drugs that affect electrolyte handling can also help keep sodium stable.
For patients with chronic kidney disease, the interplay between hyponatremia and residual renal function is especially tight.
Small improvements in sodium can translate to better blood pressure control and less stress on the new graft.
In short, keeping an eye on sodium isn’t just a lab number – it’s a proactive move to protect graft survival.
So if you or a loved one is on the transplant list, ask the transplant team to review any hyponatremia and get a clear plan in place.
Kyah Chan
October 8, 2025 AT 18:56The presented calculator, while aesthetically pleasing, suffers from a lack of methodological transparency. It fails to disclose the weighting algorithm behind symptom scoring, which raises concerns about its clinical validity. Moreover, the reliance on a binary symptom checklist oversimplifies a complex electrolyte disorder. Until peer‑reviewed validation data are made available, clinicians should treat this tool as illustrative rather than diagnostic.
Joy Arnaiz
October 8, 2025 AT 19:06One cannot ignore the shadowy influence of pharmaceutical financing behind the glossy interface of this assessment tool. The subtle push to label mild hyponatremia as merely 'monitoring' conveniently aligns with profit‑driven agendas to sell high‑margin IV fluids. While the text warns against rapid correction, it omits the fact that many hospitals have contracts incentivizing the use of expensive hypertonic solutions. The message is clear: keep patients dependent on the system, not empowered to question it.
Ananthu Selvan
October 8, 2025 AT 19:16This thing is useless stop wasting time.
Nicole Chabot
October 8, 2025 AT 19:26I’m curious how often transplant centers actually integrate a hyponatremia correction protocol into their pre‑op checklist. It would be great to see real‑world data on graft outcomes linked to pre‑operative sodium levels. Does anyone have experience with a specific protocol that works well?
Sandra Maurais
October 8, 2025 AT 19:36The calculator’s logical framework appears to be an oversimplified heuristic rather than a robust predictive model. Its binary symptom approach neglects the nuanced spectrum of neuro‑cognitive manifestations associated with electrolyte disturbances. Consequently, the risk stratification may mislead clinicians into either over‑treating or under‑treating patients. 🧐🚫
Michelle Adamick
October 8, 2025 AT 19:46Whoa, this tool is a total game‑changer for drip‑management! 🚀 Leveraging real‑time sodium telemetry can turbo‑boost graft viability metrics. Just remember to calibrate the biofeedback loop to avoid iatrogenic osmotic shifts. Let’s sync up the transplant pathway with precision electrolytics! 💡🔬
Edward Glasscote
October 8, 2025 AT 19:56Sounds legit.
Gaurav Joshi
October 8, 2025 AT 20:06Honestly, any calculator is better than guessing, but this one feels like a gimmick.
Jennifer Castaneda
October 8, 2025 AT 20:16While the inquisitiveness displayed is commendable, it is essential to acknowledge that many published protocols are curated by entities with vested interests in maintaining a dependency on proprietary correction kits. Empirical evidence suggests that independent monitoring regimens, free from such commercial bias, yield statistically superior graft survival rates. Therefore, any discussion of protocol efficacy should be grounded in data sourced from non‑conflicted research institutions.
Annie Eun
October 8, 2025 AT 20:26Sandra, your critique hits the nail on the head, yet the drama lies in the untold stories of patients whose lives hinge on these numbers. Imagine a scenario where a slight oversight in sodium assessment triggers a cascade of rejection episodes-pure nightmare material! Could we not demand a more holistic, patient‑centered algorithm that embraces the chaos of real life rather than a sterile checklist? The stakes are too high for complacency.