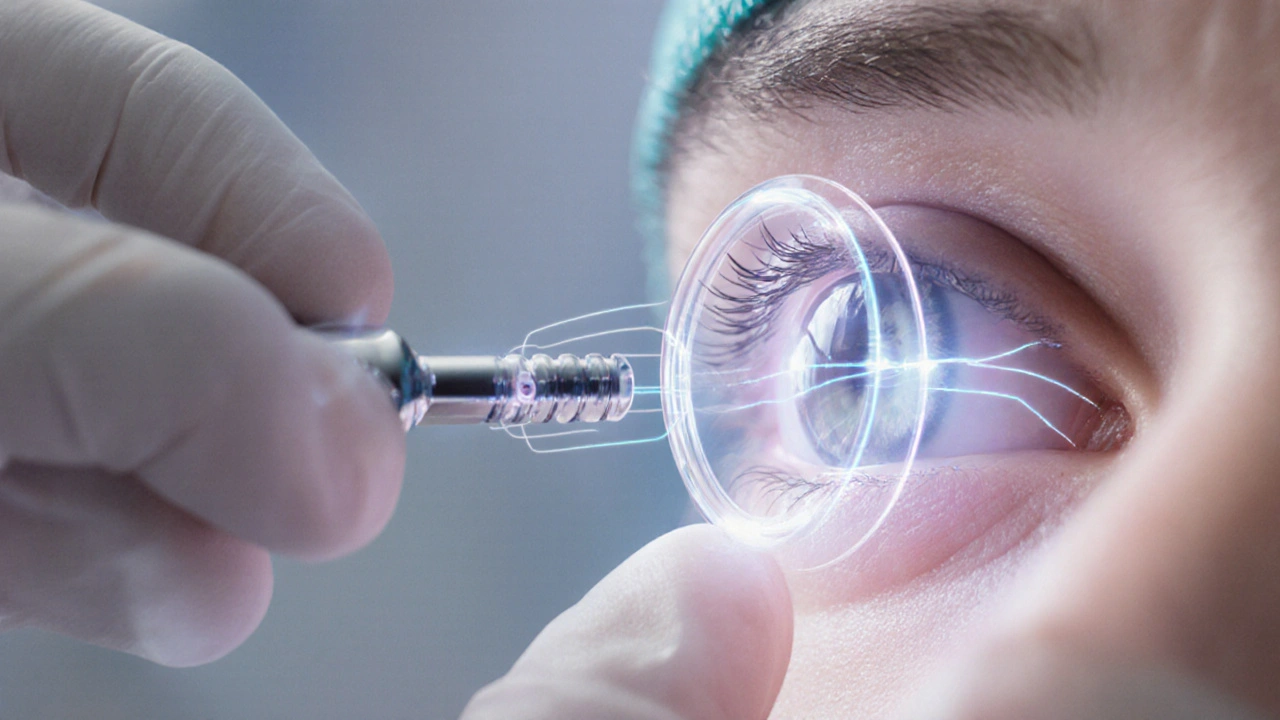
Intraocular lens is a synthetic, biocompatible implant placed inside the eye to replace the natural crystalline lens after cataract removal or refractive surgery. Designed to sit securely in the capsular bag, modern IOLs come in monofocal, toric and multifocal versions, each tuned for specific visual goals.
Why Open‑Angle Glaucoma Needs a Fresh Look
Open‑angle glaucoma is a chronic optic‑nerve disease characterized by progressive loss of retinal ganglion cells, often linked to elevated intraocular pressure (IOP). The condition silently erodes the visual field, and around 70% of glaucoma patients worldwide present with the open‑angle subtype.
Traditional management focuses on IOP control through eye drops or laser trabeculoplasty. However, medication adherence drops below 50% after two years, and laser outcomes can be unpredictable. Surgeons therefore look for combined procedures that tackle both cataract and pressure in one go.
How an IOL Helps Lower Eye Pressure
When a cataract is removed via phacoemulsification, the ultrasonic tip fragments the cloudy lens, creating space in the anterior segment. Inserting an IOL after this step has two side‑effects that benefit glaucoma:
- Deepening of the anterior chamber widens the trabecular meshwork, improving aqueous outflow.
- The newly formed capsular bag offers a stable platform for adjunctive minimally invasive glaucoma surgery (MIGS) devices.
Studies from the European Glaucoma Society (2023) report average IOP reductions of 4‑6mmHg after combined phaco‑IOL + MIGS, even without medication.
Key Surgical Pairings with Intraocular Lenses
Below are the most common ways surgeons integrate IOLs into glaucoma care.
- Phacoemulsification + IOL + MIGS - Devices such as the iStent or Hydrus are implanted into Schlemm’s canal through the same corneal incision.
- Phacoemulsification + IOL + Trabeculectomy - Traditional filtering surgery follows lens removal, offering larger IOP drops for advanced disease.
- Clear‑lens extraction + IOL - In younger patients with high‑pressure glaucoma but no cataract, the natural lens is removed to achieve a deeper anterior chamber, then a premium IOL restores vision.
Each approach balances IOP reduction, visual acuity gain and recovery time.
Clinical Outcomes: Numbers That Matter
Recent multi‑centre trials (n=1,254 eyes) provide a clear picture:
| Procedure | Mean IOP Reduction (mmHg) | Best‑Corrected Visual Acuity Gain (logMAR) | Complication Rate (%) | Typical Recovery (weeks) |
|---|---|---|---|---|
| Phaco + IOL + iStent | 5.2 | -0.15 | 4.1 | 2‑3 |
| Phaco + IOL + Hydrus | 6.0 | -0.14 | 5.3 | 2‑4 |
| Phaco + IOL + Trabeculectomy | 9.8 | -0.12 | 12.7 | 4‑6 |
All three groups showed statistically significant improvement in visual acuity, but the trabeculectomy combo delivered the deepest pressure drop at the cost of higher complication rates and longer healing.

Choosing the Right Patient
Patient selection hinges on a few core variables:
- Disease stage - Early‑to‑moderate open‑angle glaucoma benefits most from MIGS; advanced cases may need trabeculectomy.
- Lens status - Presence of a cataract or lens opacity pushes toward phaco‑IOL; a clear lens calls for “clear‑lens extraction”.
- Anterior chamber depth - Shallower chambers limit space for MIGS devices, sometimes favouring trabeculectomy.
- Corneal endothelial health - Low endothelial cell counts raise the risk of postoperative edema, influencing the decision to avoid extensive surgery.
When these factors align, a surgeon can plan a targeted approach that maximizes IOP control while restoring clear vision.
Potential Pitfalls and How to Manage Them
Even the best‑planned surgery can hit snags. Common issues include:
- Posterior capsular opacification (PCO) - A clouding behind the IOL that may require YAG laser capsulotomy.
- Endothelial cell loss - Particularly in eyes with shallow chambers; surgeons mitigate this by using dispersive viscoelastics.
- IOL dislocation - Rare but more likely after extensive capsular manipulation; proper bag fixation and choosing a stable IOL design reduce risk.
- Persistent IOP elevation - If MIGS fails, a secondary procedure or medication may be needed.
Vigilant postoperative monitoring, especially of visual field tests and optic‑nerve imaging, catches early warning signs.
Future Horizons: Smart Lenses and Beyond
Research labs are engineering IOLs that release glaucoma‑lowering drugs over months, essentially turning the lens into a slow‑release reservoir. Another frontier is adjustable‑power IOLs that can be fine‑tuned post‑operatively with a brief laser flash, ensuring perfect refraction after the eye settles.
Artificial‑intelligence algorithms are already improving lens power calculation by factoring corneal biomechanics and axial length nuances, which translates into sharper outcomes for combined surgeries.
Related Concepts Worth Exploring
While this article focuses on IOLs, readers often ask about adjacent topics such as:
- Glaucoma drainage devices (e.g., Ahmed, Baerveldt)
- Selective laser trabeculoplasty (SLT) as a non‑surgical adjunct
- Phaco‑IOL implantation in narrow‑angle eyes after laser iridotomy
- Posterior chamber vs anterior chamber IOL designs
Understanding these can help you see the full treatment landscape and decide when a lens‑centric approach fits your goals.

Frequently Asked Questions
Can an intraocular lens alone treat glaucoma?
No. An IOL replaces the natural lens but does not directly lower intraocular pressure. It becomes therapeutic when combined with cataract removal and a pressure‑lowering procedure such as MIGS or trabeculectomy.
Is MIGS safe for patients with thin corneas?
Generally yes. MIGS devices are implanted through a tiny corneal incision that spares the corneal stroma, making them suitable for eyes with fragile corneas. Surgeons still assess endothelial cell counts pre‑operatively.
What is the recovery time after phaco‑IOL plus iStent?
Most patients resume normal activities within 2‑3 weeks. Vision often stabilises by week four, and IOP readings become reliable after the first postoperative month.
Do I need glasses after a multifocal IOL?
Multifocal IOLs aim for distance and near vision without glasses, but some patients still need glasses for fine print or low‑light activities. A small prescription boost is common.
How often should I have follow‑up after combined surgery?
Typical schedule: day‑1, week‑1, month‑1, then every 3‑6 months for the first two years. Additional visits are added if IOP spikes, inflammation, or visual changes occur.




Dustin Hardage
September 27, 2025 AT 16:48The integration of intraocular lenses (IOLs) into glaucoma surgery represents a logical extension of modern cataract practice. By deepening the anterior chamber, an IOL creates additional space for aqueous outflow, which can translate into measurable pressure reductions. Recent European Glaucoma Society data show average IOP drops of 4‑6 mmHg when phaco‑IOL is combined with MIGS devices. Moreover, the stable capsular bag provides an ideal platform for adjunctive implants without increasing surgical trauma. Patients who undergo phaco‑IOL plus iStent typically achieve visual acuity gains of –0.15 logMAR while reducing medication burden. The approach also shortens recovery time compared with standalone trabeculectomy, making it attractive for early‑to‑moderate disease. In summary, the evidence supports IOL‑assisted procedures as a cost‑effective, vision‑preserving option for many open‑angle glaucoma patients.
Dawson Turcott
October 1, 2025 AT 04:08Wow, so we just slapp an extra lens in and hope the pressure drops? 🤔 Guess the eye’s a magic trick bag now. lol, but hey, if it works, why not.
Alex Jhonson
October 4, 2025 AT 15:28Just a heads‑up for anyone considering clear‑lens extraction: make sure your corneal endothelial count is solid, otherwise you might end up with post‑op edema that drags you back into the clinic. Also, a toric IOL can correct mild astigmatism that often shows up after cataract removal, which is a nice bonus for patients with glaucoma who need sharp vision for daily tasks. Keep an eye on the anterior chamber depth – too shallow and the MIGS device could hit the iris. Simple checks go a long way.
Katheryn Cochrane
October 8, 2025 AT 02:48Honestly, this whole “one‑size‑fits‑all” hype feels like a marketing ploy. The complication rate for phaco‑IOL plus trabeculectomy sits at over 12 %, which is not negligible. And let’s not forget posterior capsular opacification – a delayed problem that adds another laser session. If you’re just chasing mild IOP numbers, a simple laser trabeculoplasty could be safer.
Michael Coakley
October 11, 2025 AT 14:08So we’re basically playing Jenga with the eye, stacking lenses and stents, hoping it doesn’t tumble. The philosophy is cute, but the reality is that every additional device adds another point of failure. Still, for some patients the trade‑off might be worth it.
ADETUNJI ADEPOJU
October 15, 2025 AT 01:28From a device‑integration standpoint, the synergistic effect of a phaco‑IOL scaffold and a micro‑invasive trabecular bypass can be modeled using fluid‑dynamic simulations that predict a modest 5‑10 % increase in outflow facility. While the literature touts “significant” pressure drops, a passive interpretation suggests the incremental benefit may be marginal when baseline IOP is already low. Nonetheless, the jargon‑laden narrative underscores the trend toward minimally invasive multimodal therapy.
Janae Johnson
October 18, 2025 AT 12:48It is often overlooked that the cost implications of combined procedures can outweigh the modest IOP gains, especially in health systems with limited resources. Moreover, the notion that a lens implant can substitute for pharmacologic control is, at best, an overstatement.
Kayla Charles
October 22, 2025 AT 00:08While I appreciate the cautionary tone, I must emphasize that the collective body of evidence actually paints a more nuanced picture. First, the randomized trials cited in the article encompass a diverse patient cohort, ranging from early-stage to advanced glaucoma, which demonstrates the versatility of IOL‑based strategies. Second, the visual acuity improvements reported are not merely statistical artifacts; they translate into real‑world functional benefits such as improved reading speed and reduced dependency on glasses. Third, the complication profile, although higher in trabeculectomy combos, remains within acceptable limits when surgeons adhere to meticulous technique and postoperative monitoring. Fourth, the advent of premium IOL designs, including toric and multifocal models, addresses residual astigmatism and presbyopia, thereby enhancing overall patient satisfaction. Fifth, the emerging field of drug‑eluting IOLs holds promise for sustained IOP control without the need for additional implants. Sixth, artificial‑intelligence‑driven lens power calculations are reducing refractive surprises, which historically have been a deterrent to combining procedures. Seventh, patient‑reported outcome measures consistently favor combined surgery over staged interventions, citing convenience and reduced anxiety. Eighth, from a health‑economics perspective, a single operative episode diminishes cumulative costs associated with multiple clinic visits, medication refills, and potential emergency interventions. Ninth, the learning curve for MIGS devices attached to IOLs is relatively short for seasoned cataract surgeons, facilitating wider adoption. Tenth, postoperative inflammation can be effectively managed with a brief course of topical steroids, limiting long‑term complications. Eleventh, the role of clear‑lens extraction in younger patients should not be dismissed; it expands the therapeutic arsenal for those with high‑pressure glaucoma but minimal cataract formation. Twelfth, the collaborative approach between cornea, glaucoma, and cataract specialists fosters interdisciplinary expertise that ultimately benefits the patient. Thirteenth, long‑term data beyond five years are still emerging, yet early trends suggest durability of IOP reduction. Fourteenth, patient education remains paramount; informed individuals are more likely to adhere to follow‑up schedules, which mitigates the risk of delayed pressure spikes. Finally, the future of IOL‑centric glaucoma management looks promising, with ongoing research into adjustable‑power lenses and bio‑compatible drug delivery platforms that could redefine the standard of care.
Paul Hill II
October 25, 2025 AT 11:28From a practical standpoint, the decision matrix for choosing between MIGS and trabeculectomy hinges on the surgeon’s comfort level and the patient’s disease severity. In my experience, patients with moderate open‑angle glaucoma appreciate the quicker visual recovery after a phaco‑IOL plus iStent, while those with advanced damage often need the larger pressure drop that trabeculectomy provides.
Stephanie Colony
October 28, 2025 AT 21:48Honestly, the so‑called “cutting‑edge” IOL combos are just a way for the industry to cash in on hype. If you ask me, the classic trabeculectomy still reigns supreme for true pressure control.
Abigail Lynch
November 1, 2025 AT 09:08Ever wonder why the big pharma giants are suddenly pushing these lens implants? Some say it’s a coordinated effort to divert attention from the fact that many glaucoma drugs are being phased out in favor of surgical revenues. The whole thing smells like a carefully orchestrated plot to keep patients dependent on high‑tech solutions.
David McClone
November 4, 2025 AT 20:28Sure, a lens can help, but it won’t magically cure glaucoma.