Narrow therapeutic index drugs aren’t just another type of medicine. They’re the kind where a tiny change in your dose - even as small as a fraction of a pill - can mean the difference between getting better and ending up in the hospital. These drugs have a razor-thin safety margin. Too little, and they don’t work. Too much, and they can cause serious harm or even death.
Why NTI Drugs Are Different
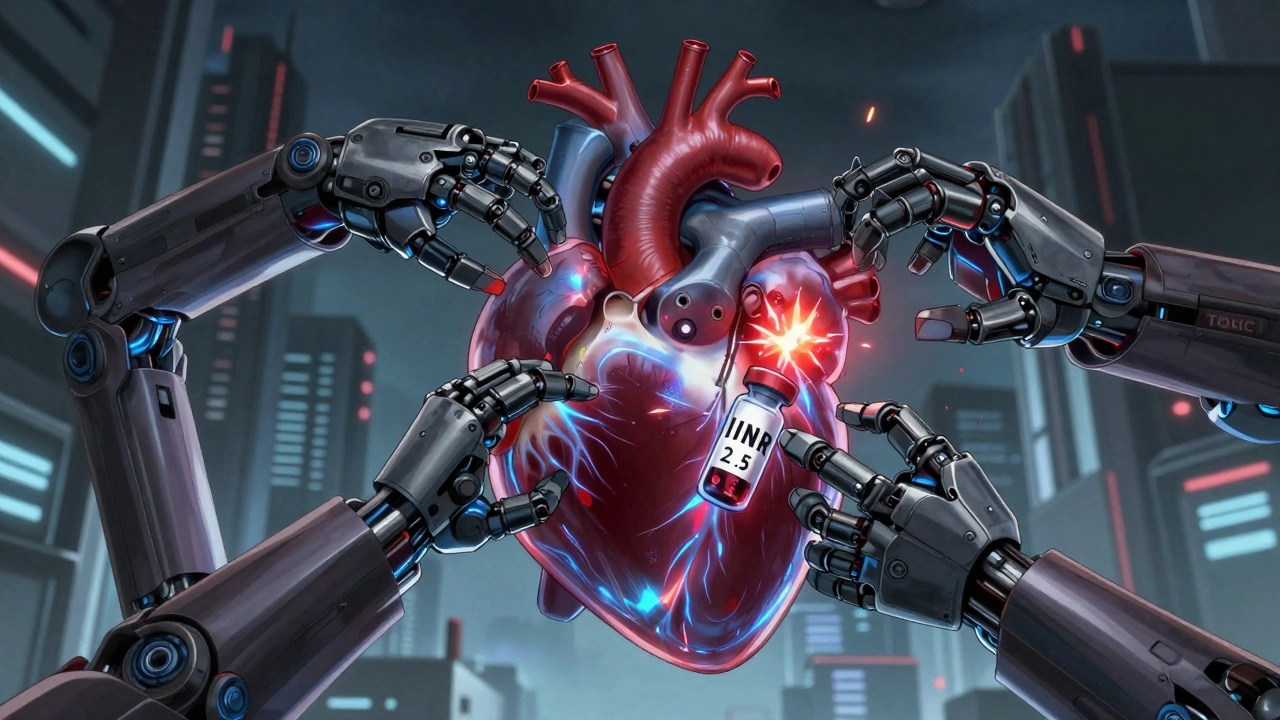
Most medications have a wide safety zone. If you take a little more or less than prescribed, your body can usually handle it without major issues. That’s not true for narrow therapeutic index drugs. The gap between the dose that helps you and the dose that hurts you is extremely small - often less than double. For example, with warfarin, your blood needs to stay within a very tight range (INR 2.0-3.0) to prevent clots without causing bleeding. Go above 3.5, and your risk of dangerous bleeding skyrockets.This isn’t theoretical. In real life, patients have ended up in emergency rooms after switching from one generic version of an NTI drug to another. One woman on warfarin saw her INR jump from 2.5 to 4.1 after her pharmacy switched her to a different generic brand. She needed emergency treatment to stop the bleeding. That’s not rare. Studies show patients who switch between different generic versions of NTI drugs are more than twice as likely to be hospitalized for complications.
Common NTI Drugs You Might Be Taking
You might already be on one of these without realizing it. Here are the most common narrow therapeutic index drugs:- Warfarin (Coumadin, Jantoven) - Used to prevent blood clots. Requires frequent blood tests (INR) to monitor.
- Lithium (Lithobid) - Treats bipolar disorder. Toxicity can cause tremors, confusion, seizures. Blood levels must stay between 0.6-1.2 mmol/L.
- Levothyroxine (Synthroid) - Replaces thyroid hormone. Even small changes in dose can cause fatigue, weight gain, or heart problems.
- Digoxin (Lanoxin) - Helps with heart failure and irregular heartbeat. Levels above 2.0 ng/mL can cause life-threatening heart rhythms.
- Tacrolimus (Prograf) - Used after organ transplants. Too low = organ rejection. Too high = kidney damage.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol) - Seizure medications. Small changes can trigger seizures or cause dizziness, nausea, and even coma.
- Methotrexate (Trexall) - Used for autoimmune diseases and some cancers. Overdose can damage your liver and bone marrow.
These aren’t just “strong” drugs - they’re drugs that demand precision. A 10% change in blood concentration can push you from safe to dangerous. That’s why your doctor doesn’t just write a prescription and send you on your way.
Monitoring Is Non-Negotiable
If you’re on an NTI drug, regular blood tests aren’t optional. They’re your safety net.For warfarin, you might need an INR test every week at first, then every few weeks once your dose is stable. Lithium levels are checked every 3-6 months - or more often if your dose changes. After a kidney transplant, tacrolimus levels are checked twice a week initially. These aren’t just routine visits - they’re life-saving checks.
Why? Because your body doesn’t process these drugs the same way every day. Food, other medications, even stress or illness can change how much of the drug gets into your bloodstream. A cold, a new antibiotic, or skipping a meal can throw off your levels. That’s why consistency matters more than you think.
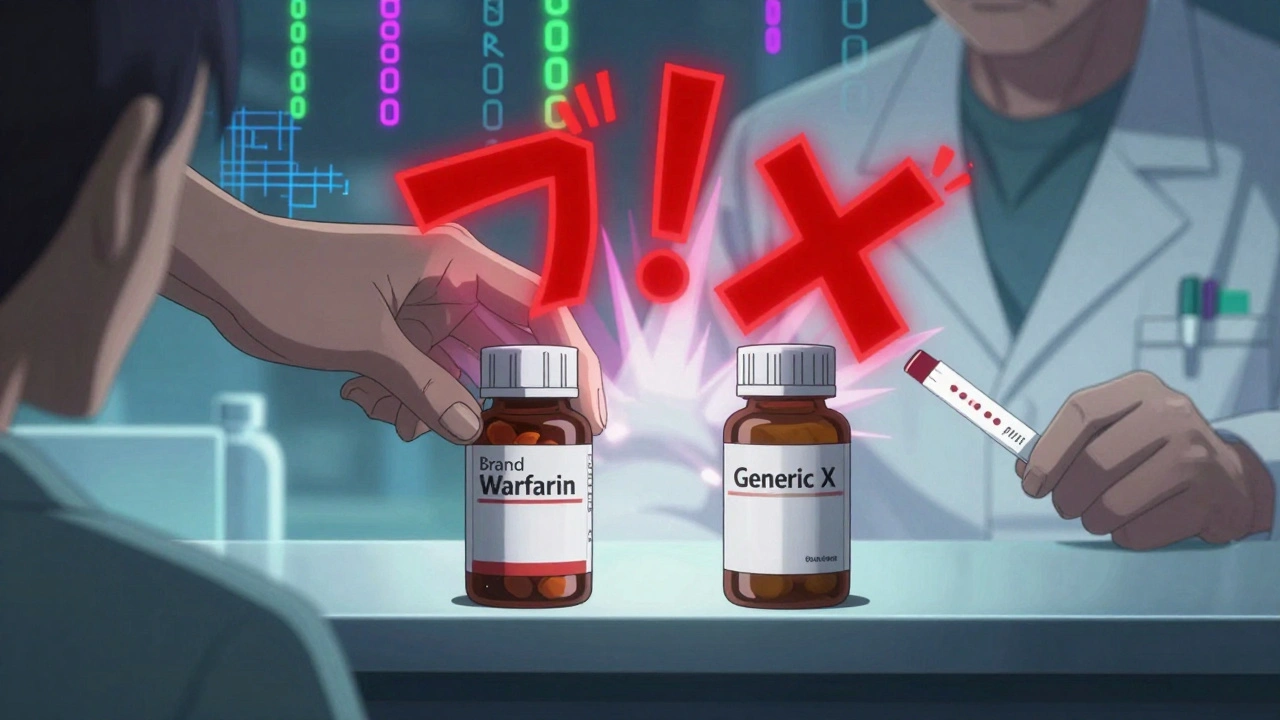
Don’t Switch Brands - Even If It’s “The Same”
You’ve probably heard that generic drugs are just as good as brand-name ones. That’s usually true - but not for NTI drugs.The FDA allows generic drugs to be 80-125% as potent as the brand version. For most drugs, that’s fine. But for NTI drugs, that’s too wide. A 25% difference in absorption could push your lithium level from 1.0 to 1.25 - still in the “normal” range - but enough to trigger side effects. Or worse, it could drop your tacrolimus level from 12 to 9, putting your new organ at risk of rejection.
That’s why the European Medicines Agency requires generics of NTI drugs to be within 90-111% of the brand - a much tighter range. In the U.S., some states like North Carolina require pharmacists to get your doctor’s permission before switching your NTI drug to a different generic. Always ask your pharmacist: “Is this the same brand I’ve been taking?” If they say yes, great. If they say “it’s just a different generic,” ask your doctor first.
What Happens If You Miss a Dose or Take Too Much?
Missing a dose of an NTI drug can be just as dangerous as taking too much.With levothyroxine, skipping a dose for a few days can make you feel sluggish, gain weight, or get cold easily - signs your thyroid levels are dropping. With warfarin, missing doses increases your risk of clots, which could lead to a stroke or pulmonary embolism.
On the flip side, taking an extra pill of lithium could cause vomiting, diarrhea, shaking, or confusion. An extra dose of digoxin could trigger a dangerous heart rhythm. These aren’t side effects you can “wait out.” They need immediate medical attention.
If you accidentally take too much, call your doctor or go to the ER. Don’t wait. If you miss a dose, don’t double up the next day. Call your provider for instructions.
How to Stay Safe Every Day
Managing an NTI drug takes work - but it’s manageable. Here’s how:- Use the same pharmacy every time. They’ll keep your records consistent and flag potential switches.
- Keep a medication log. Write down your dose, any side effects, and when you had blood tests. Patients who do this have 32% fewer problems.
- Know the signs of toxicity and under-dosing. For lithium: tremors, confusion, frequent urination. For warfarin: unusual bruising, nosebleeds, dark stools. For levothyroxine: fatigue, weight gain, depression.
- Tell every doctor you see you’re on an NTI drug. Even your dentist needs to know - some antibiotics and painkillers can interfere.
- Don’t start supplements without checking. St. John’s wort, vitamin K, and even grapefruit juice can mess with your levels.
- Set phone reminders. For doses and blood tests. Don’t rely on memory.
What’s Changing in the Future
The FDA is working on a new system to officially list which drugs are NTI - something they’ve avoided doing for years. By 2024, they plan to release a clear, public list. That means more transparency for patients and pharmacists.Also, genetic testing is becoming part of the picture. For warfarin, your genes (CYP2C9 and VKORC1) can explain up to 60% of why you need a higher or lower dose. Some hospitals already test for this before starting treatment. By 2026, this could become standard for several NTI drugs, making dosing more accurate from day one.
Apps are also helping. The FDA has cleared three mobile apps that let you log your doses, track symptoms, and remind you when to get blood work. These aren’t just gadgets - they’re tools that reduce risk.
You’re Not Alone
It’s overwhelming at first. But thousands of people manage NTI drugs successfully every day. One man on Reddit shared that after switching to consistent lithium monitoring, he went from three hospitalizations in two years to zero in eight. Another woman on a thyroid forum said her energy returned within weeks after sticking to the same brand of levothyroxine.It’s not about being perfect. It’s about being consistent. About knowing your numbers. About asking questions. About speaking up when something feels off.
If you’re on one of these drugs, you’ve already taken the most important step: you’re paying attention. Keep going. Your life depends on it - and you’ve got this.
What does "narrow therapeutic index" mean?
It means the difference between a safe, effective dose and a harmful or toxic dose is very small. Even a slight change in how much you take - or how your body absorbs it - can lead to serious side effects or make the drug stop working.
Can I switch between generic brands of my NTI drug?
It’s not recommended. Even though generics are supposed to be the same, small differences in how they’re made can change how much of the drug enters your bloodstream. For NTI drugs, that can be dangerous. Always check with your doctor before switching.
How often do I need blood tests?
It depends on the drug. Warfarin patients usually get INR tests every 1-4 weeks. Lithium levels are checked every 3-6 months after stabilization. Tacrolimus requires frequent testing right after a transplant - sometimes twice a week. Your doctor will tell you your schedule based on your condition and how stable your levels are.
What should I do if I miss a dose?
Don’t double up. Contact your doctor or pharmacist immediately. For some NTI drugs like levothyroxine, missing one dose isn’t an emergency - but missing several can cause symptoms. For others like warfarin or lithium, missing doses can be risky. Always follow professional advice.
Are there apps to help manage NTI drugs?
Yes. The FDA has approved three mobile apps that help patients track doses, symptoms, and lab results for NTI drugs. These tools can reduce errors and help you stay on schedule. Ask your pharmacist or doctor for recommendations.
Can other medications or foods affect my NTI drug?
Absolutely. Antibiotics, antifungals, seizure meds, and even grapefruit juice can interfere. Vitamin K affects warfarin. Salt and hydration affect lithium. Always tell every provider you see what you’re taking - including supplements and over-the-counter drugs.
Next Steps If You’re on an NTI Drug
Start today. Make a list of every NTI drug you take. Write down your current dose and when your next blood test is due. Call your pharmacy and ask if you’ve been on the same brand consistently. If not, talk to your doctor about sticking with one. Download a medication tracker app. Print out a symptom checklist for your drug. Keep it in your wallet.You don’t need to be an expert. You just need to be informed, consistent, and proactive. That’s how people stay safe with these powerful medicines - and you can too.



zac grant
December 4, 2025 AT 19:46NTI drugs are wild. One tiny slip and you're in the ER. I've been on warfarin for 5 years and my INR's been stable as hell since I stuck to the same pharmacy and never switched generics. The blood tests suck, but they're cheaper than a hospital bill.
Pro tip: Use a pill organizer with alarms. I set mine for 8 AM and 8 PM. No excuses. Also, keep a little card in your wallet with your meds and emergency contact. First responders appreciate it.
And yeah, grapefruit juice? Avoid it like the plague. It messes with CYP3A4 and turns your tacrolimus into a landmine.
Heidi Thomas
December 6, 2025 AT 02:15Stop pretending generics are dangerous. The FDA approves them. If your doctor can't manage your levels properly that's on them not the pharmacy. I've switched generics 12 times on lithium and never had an issue. People are paranoid because they don't understand pharmacokinetics. Stop fearmongering.
Jordan Wall
December 7, 2025 AT 10:38Actually, the EMA's 90–111% bioequivalence range for NTIs is the only scientifically defensible standard. The FDA's 80–125% is a relic of 1980s regulatory laziness. I mean, c'mon - we're talking about drugs where a 10% fluctuation can trigger arrhythmias or transplant rejection. This isn't ibuprofen.
Also, did you know that some generics use different fillers like lactose monohydrate vs. microcrystalline cellulose? That alters dissolution kinetics. 🤓
PS: I'm a clinical pharmacologist. You're welcome.
Isabelle Bujold
December 9, 2025 AT 04:34It's important to recognize that the variability in generic NTI drugs isn't just about potency - it's about consistency in absorption over time. Some patients have slower gastric emptying or altered gut flora due to antibiotics or even probiotics, which can make even a 'within-range' generic behave unpredictably in their system. That's why the recommendation to stay on one brand isn't just caution - it's personalized medicine in action.
And yes, I've seen patients on levothyroxine whose TSH levels fluctuated wildly after a pharmacy switch, only to stabilize within weeks of returning to the original brand. It's not placebo. It's pharmacology.
Also, don't underestimate the psychological impact. When patients know they're on the same formulation, they're more likely to adhere to monitoring schedules. Trust matters as much as chemistry.
John Filby
December 9, 2025 AT 06:26Just wanna say thanks for this post - I'm on tacrolimus after my kidney transplant last year and I didn't realize how much detail goes into this stuff. I started using the FDA-approved med tracker app and it actually helped me catch a dose I missed last week before my blood test. My nurse said my levels were the most stable they've been in months 😅
Also, I switched to one pharmacy and they literally call me before refilling if they think it's a different generic. Lifesaver.
Elizabeth Crutchfield
December 9, 2025 AT 12:09i was on warfarin for afib and i switched generics once and got a nosebleed that lasted 3 hours. never again. now i use the same pharmacy, same brand, and i even take my pill at the same time every day. no jokes. this shit is serious. 🙏
Ashley Elliott
December 10, 2025 AT 17:00For anyone new to NTI drugs: it's okay to feel overwhelmed. You're not lazy for needing reminders, charts, or help. This isn't about discipline - it's about designing systems that account for human error. I keep a laminated card with my drug, target range, and emergency contacts in my purse. My mom keeps a copy in her phone. We check in every Sunday.
And if your doctor dismisses your concerns about generics? Find a new one. Your life is worth more than a $5 savings.
Augusta Barlow
December 11, 2025 AT 06:22Let me ask you something - why do you think the FDA still allows 80–125% variability for NTI drugs? Have you ever looked into the lobbying behind generic manufacturers? The same companies that make the brand versions also make the generics. It's a conflict of interest disguised as 'affordability'.
And don't get me started on those 'FDA-approved' apps. They're data mines. Your medication history, your blood results, your habits - all feeding into some algorithm that insurers will use to raise your premiums. They're not helping you. They're profiling you.
Stay off the apps. Write it down on paper. Burn the digital trail.
Joe Lam
December 12, 2025 AT 02:20Wow. So let me get this straight - you're telling people to avoid generics because some pharmacist might switch them? That's like saying you shouldn't drive because some idiot might run a red light. If your doctor can't adjust your dose for bioavailability differences, they shouldn't be prescribing NTI drugs. This post is fear porn wrapped in pseudoscience.
Jenny Rogers
December 13, 2025 AT 13:15One cannot help but observe the profound epistemological rupture in contemporary pharmacological discourse. The notion that a patient's autonomy can be meaningfully preserved through institutionalized monitoring protocols - rather than through the cultivation of self-reflective vigilance - is a symptom of late-stage biomedical reductionism.
Indeed, the very premise of the narrow therapeutic index implies a metaphysical fragility in the human organism, one that cannot be calibrated by algorithmic reminders or pharmacy loyalty programs. True safety lies not in adherence, but in ontological humility before the pharmakon.
-Jenny Rogers, Ph.D. in Medical Philosophy
Scott van Haastrecht
December 13, 2025 AT 14:40My sister died from a digoxin overdose after her pharmacy switched her generic. They didn't even tell her. She was 42. They call it 'cost-saving'. I call it murder by bureaucracy.
Now I go to court every time a pharmacy tries to switch my meds. I've sued three pharmacies. I've won every case. If you're on an NTI drug, don't trust anyone. Not your doctor. Not your pharmacist. Not the FDA. Call your prescriber yourself. Every. Single. Time.
And if you're still using an app? Delete it. They're watching you.