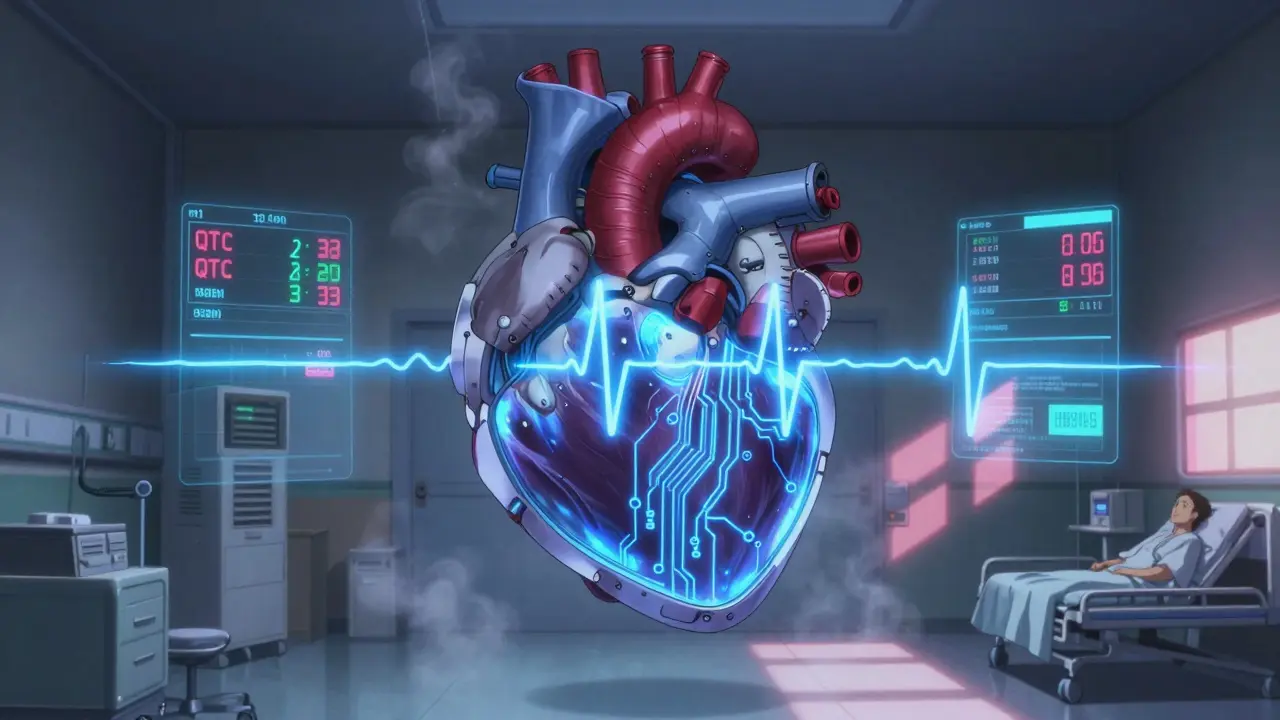
Macrolide QT Risk Calculator
This tool helps you assess your risk of QT prolongation when taking macrolide antibiotics like azithromycin, clarithromycin, or erythromycin. Based on the 2025 AHA guidelines, a score of 4 or higher indicates elevated risk.
Risk Assessment Result
Your risk of QT prolongation with macrolide therapy is low.
Points System: 1 point for each risk factor (except drug type)
Drug type points: Erythromycin = 2 points, Clarithromycin = 1 point, Azithromycin = 0 points
Score of 4 or higher indicates elevated risk requiring ECG monitoring
When you’re prescribed an antibiotic like azithromycin or clarithromycin for a stubborn chest infection, you probably don’t think about your heart. But here’s the thing: these common drugs can mess with your heart’s electrical rhythm. Not often. Not in everyone. But enough that doctors need to know who’s at real risk - and who doesn’t need an ECG before starting treatment.
Why Macrolides Can Be Risky for Your Heart
Macrolide antibiotics - azithromycin, clarithromycin, erythromycin - work great against pneumonia, bronchitis, and sinus infections. But they also block a specific potassium channel in heart cells called hERG. That’s not a problem for most people. But for some, it slows down the heart’s recovery phase after each beat. On an ECG, that shows up as a longer QT interval. And when that interval gets too long, it can trigger a dangerous rhythm called Torsades de Pointes - a type of ventricular arrhythmia that can lead to sudden cardiac arrest.
The risk isn’t huge overall. About 1 to 8 cases of Torsades happen per 10,000 people taking macrolides each year. But that number jumps sharply if your QTc (corrected QT interval) is above 500 milliseconds. For every 10 ms above that, your risk goes up by 5-7%. Erythromycin carries the highest risk, followed by clarithromycin. Azithromycin is lower, but still not zero - especially if you’re already at risk.
Who Should Get an ECG Before Taking Macrolides?
The British Thoracic Society says: everyone getting long-term macrolide therapy - think months for bronchiectasis or cystic fibrosis - should have a baseline ECG. That’s because these patients are often on the drug for weeks or longer, and the risk builds up over time.
But here’s the real question: what about someone getting a 5-day course of azithromycin for a bad cough? Do they need an ECG too?
The answer isn’t yes or no - it’s who. According to experts, you need an ECG if you have any of these risk factors:
- Female sex - women are nearly three times more likely to develop drug-induced QT prolongation
- Age 65 or older - risk doubles after 65
- Already taking other QT-prolonging drugs - like certain antidepressants, antifungals, or antiarrhythmics
- History of heart disease, heart failure, or prior arrhythmia
- Low potassium or magnesium levels - common in people on diuretics or with eating disorders
- Chronic kidney disease - especially stage 3 or worse
- Family history of sudden cardiac death or Long QT Syndrome
- Already have a QTc over 450 ms in men or 470 ms in women
That’s it. You don’t need an ECG just because you’re getting a macrolide. But if you have one or more of these, you absolutely should.
What Do Guidelines Actually Say?
There’s a big gap between what guidelines recommend and what actually happens in clinics.
The British Thoracic Society (BTS) has clear rules: baseline ECG before long-term macrolide use, then another at one month. In specialized respiratory clinics in the UK, 87% follow this. But in regular GP offices? Only 12% do.
Why? Time. Cost. Uncertainty.
An ECG costs around £28.50 in the UK. With over 12 million macrolide prescriptions issued annually, universal screening would cost £342 million a year. That’s not feasible. And most GPs aren’t trained to interpret borderline QTc values - say, 470-499 ms - which are tricky. One misread, and you might miss a dangerous case.
Meanwhile, the American Heart Association and NIH now support a risk-stratified approach. That means you don’t screen everyone - you screen the people who are most likely to have problems. The 2025 update to the AHA guidelines introduced a 9-point scoring system that weighs age, sex, kidney function, and drug interactions. If your score is 4 or higher, get the ECG. If it’s lower, you’re probably fine.
What Happens If You Skip the ECG?
Most people will be fine. But some won’t.
There’s a documented case from a Reddit thread in March 2025: a 68-year-old woman with no known heart issues, QTc of 480 ms at baseline, took clarithromycin for pneumonia. Five days later, she went into Torsades de Pointes. Emergency cardioversion saved her life. She had never had an ECG before. Her doctor assumed she was healthy - and she was, except for one hidden risk: she was on a diuretic and had borderline low potassium.
That’s the problem. Risk factors aren’t always obvious. A patient might not mention their old diuretic. Or they might not know their dad died suddenly at 52. That’s why screening isn’t about suspicion - it’s about catching the silent risks.
On the flip side, mandatory screening in respiratory clinics found that 1.2% of patients had previously undiagnosed Long QT Syndrome. That’s one in 80 people. Without screening, they’d have been prescribed macrolides - and might not have survived.
How Is This Done in Practice?
If you’re in a hospital or a specialist clinic, it’s straightforward. The ECG is ordered before the prescription is written. Results come back in minutes. If QTc is over 450 (men) or 470 (women), the doctor switches to a safer antibiotic - like amoxicillin or doxycycline.
In primary care? It’s messier.
A 2024 survey of 247 UK GPs showed 78% knew macrolides could prolong QT. But only 22% ordered baseline ECGs. Why? 65% said they didn’t have time. 58% said guidelines weren’t clear for short courses. 47% thought healthy patients were fine.
But here’s what’s changing: electronic health records are starting to help. Epic Systems, one of the biggest EHR platforms in the US, now flags macrolide prescriptions if the patient has risk factors - like age, kidney disease, or another QT-prolonging drug. That alert pops up right when the doctor clicks “prescribe.” It doesn’t force a decision, but it reminds them: Did you check the ECG?
In the UK, pilot programs are testing point-of-care ECG devices in respiratory clinics. These handheld machines give results in under 2 minutes. One clinic reduced the wait time for treatment from 5.2 days to 0.8 days. That’s huge.
What If Your QTc Is Borderline?
Let’s say your ECG shows a QTc of 465 ms. You’re a 52-year-old woman. No heart disease. No other meds. Just a simple chest infection.
Here’s what to do:
- Check your electrolytes - get a simple blood test for potassium and magnesium.
- Review all your other medications - even over-the-counter ones. Antihistamines like diphenhydramine can also prolong QT.
- Consider switching to a non-macrolide antibiotic if possible.
- If you must use a macrolide, avoid high doses. Azithromycin 500 mg once daily for 5 days is safer than 1 g on day one.
- Ask for a repeat ECG after 5-7 days if you’re on the drug longer than a week.
Don’t panic. But don’t ignore it either.
The Bottom Line
ECG monitoring isn’t needed for everyone on macrolides. But it’s critical for people with risk factors. The data is clear: age, sex, kidney function, other drugs, and existing heart conditions make the difference between a safe course of antibiotics and a life-threatening event.
Doctors aren’t being careless. They’re overwhelmed. But technology - automated alerts, point-of-care ECGs, risk scores - is making it easier to do the right thing without burning out.
If you’re prescribed azithromycin or clarithromycin, ask: Do I have any of these risk factors? If yes, push for an ECG. If you’re a clinician, don’t wait for guidelines to catch up. Use the 9-point risk score. Check the meds. Check the labs. It takes two minutes. And it could save a life.





Jake Moore
January 17, 2026 AT 19:49Just had a patient last week on clarithromycin with a QTc of 482. No symptoms, no history, but she was on furosemide and had a mom who dropped dead at 54. We did the ECG, switched to amoxicillin, and called it a day. This post nailed it-screening isn’t about suspicion, it’s about catching the silent risks.
Doctors aren’t lazy. We’re just drowning in alerts and paperwork. Give us tools, not guilt.
Joni O
January 19, 2026 AT 15:49Thank you for writing this. I’m a nurse and I’ve seen too many people get prescribed azithromycin like it’s cough syrup. My grandma took it for a sinus infection and ended up in the ER with a weird flutter. They didn’t check her electrolytes. She was on a diuretic and didn’t even know it.
Don’t ignore the little things. Potassium matters. Asking for an ECG isn’t being dramatic-it’s being smart.
Eric Gebeke
January 21, 2026 AT 14:49Wow. Just wow. Another one of those ‘medical professionals think they know better than patients’ posts. You act like ECGs are harmless and free. They’re not. They’re expensive, overused, and often misread. You’re basically advocating for a nationwide panic over a risk that’s statistically negligible for healthy people.
Let me guess-you also want everyone to get a CT scan before taking ibuprofen? Because that’s just as ‘dangerous’ if you stretch the data enough.
Stop fearmongering with cherry-picked case reports. The real epidemic here is overmedicalization.
Ryan Otto
January 21, 2026 AT 19:21Let’s not pretend this is about patient safety. This is about corporate profit disguised as clinical wisdom. The ECG industry, pharmaceutical giants, and EHR vendors are colluding to create artificial risk profiles. Why? Because if you can convince GPs that every 5-day azithromycin course requires a $28.50 test, you create a new revenue stream.
And don’t get me started on the ‘9-point scoring system’-it’s a statistical illusion designed to justify overtesting. The real danger? The erosion of clinical autonomy. We’re being turned into algorithm-following clerks.
Who benefits? Not the patient. Not the doctor. The system.
Max Sinclair
January 22, 2026 AT 08:27I appreciate how balanced this is. I’ve been in primary care for 12 years and I’ve seen both sides. I used to skip ECGs because I thought, ‘She’s healthy, she’s fine.’ Then I had a 71-year-old woman on lisinopril and hydrochlorothiazide take azithromycin. She had a QTc of 495-never been checked before. She coded 3 days later.
It wasn’t her fault. It wasn’t my fault. It was the system’s fault for not giving us better tools.
Now I use the AHA score. It takes 30 seconds. And I always check meds and electrolytes. Small things. Big difference.
Praseetha Pn
January 23, 2026 AT 10:08OMG you guys, this is a total mind control ploy by Big Pharma and the FDA to make us all dependent on machines! They don’t want us to heal naturally-they want us to be hooked on ECGs, labs, and pills!
My cousin in India got pneumonia and took turmeric with black pepper and garlic oil for 3 days-CURED. No ECG. No antibiotics. No hospital.
They’re scared because if people start trusting herbs, the whole profit machine collapses. And don’t even get me started on how they’re using ‘QTc’ to gaslight women into thinking our hearts are broken!
Check your vibes, not your ECG. Your body knows.
Emma #########
January 25, 2026 AT 02:50This made me think of my dad. He’s 73, on a diuretic for high blood pressure, and last year he got a 5-day course of azithromycin for bronchitis. He never mentioned he was on it until he said, ‘I felt weird, like my heart was skipping.’ We didn’t think much of it.
Reading this… I’m so glad we didn’t brush it off. I’m taking him to get his QT checked next week. Thanks for the nudge. It’s easy to ignore when you feel fine.
Andrew McLarren
January 25, 2026 AT 10:26It is imperative to underscore the clinical imperative of risk-stratified ECG screening in the context of macrolide administration. The epidemiological data, while statistically modest in absolute terms, demonstrates a non-linear increase in arrhythmic risk contingent upon the confluence of predisposing variables, including but not limited to renal insufficiency, concomitant pharmacotherapy, and sex-based electrophysiological variance.
Moreover, the integration of automated clinical decision support systems into electronic health records represents a paradigmatic advancement in preventive cardiology, mitigating cognitive load while enhancing diagnostic fidelity. The cost-benefit analysis, when viewed through the lens of preventable mortality, remains overwhelmingly favorable.
It is not overtesting. It is intelligent triage.
Andrew Short
January 27, 2026 AT 02:58Pathetic. You’re all just playing doctor with spreadsheets. This isn’t medicine-it’s fear-based billing. A 68-year-old woman with a QTc of 480 gets a heart attack because she took a 5-day antibiotic? Newsflash: she probably had undiagnosed heart disease, not ‘drug-induced’ anything.
You’re turning every healthy person into a patient. You’re creating a generation of hypochondriacs who think their heartbeat is a ticking bomb.
Stop blaming doctors. Stop pushing ECGs. Let people breathe. And for god’s sake, stop monetizing anxiety.
christian Espinola
January 28, 2026 AT 20:32So let me get this straight: we’re going to screen 12 million people for a risk that affects 1 in 10,000… but we don’t screen for the 1 in 5 who have untreated hypertension? Or the 1 in 3 with prediabetes?
This isn’t medicine. It’s performative safety. You want to save lives? Fix the healthcare access crisis. Stop chasing tiny statistical ghosts while people die waiting for insulin.
ECGs won’t fix poverty. Or loneliness. Or the fact that half the country can’t afford a primary care visit.
Save the alerts for the real emergencies.