When a patient walks into a hospital with high blood pressure, diabetes, or an infection, they don’t get to pick their medication. The drug they receive isn’t chosen by the doctor alone-it’s decided by a behind-the-scenes system called the hospital formulary. This isn’t just a list of approved drugs. It’s a living, breathing decision-making engine that balances safety, effectiveness, and cost. And at the heart of it? Generic drugs.
What Exactly Is a Hospital Formulary?
A hospital formulary is a curated list of medications that staff are allowed to prescribe and dispense. It’s not static. It’s updated every few months, sometimes weekly, based on new data, shortages, or cost shifts. Most U.S. hospitals with 100 or more beds use a closed formulary, meaning only approved drugs are routinely stocked. If a drug isn’t on the list, getting it requires special permission-a process that can delay care. The formulary isn’t managed by one person. It’s overseen by a Pharmacy and Therapeutics (P&T) committee. This group includes pharmacists, physicians, nurses, and sometimes a healthcare economist. They meet regularly to review new drugs, evaluate existing ones, and decide what stays, what goes, and what gets swapped out.Why Generics? The Cost-Effectiveness Factor
Generic drugs make up 90% of all prescriptions filled in U.S. hospitals-but only 26% of total drug spending. That’s the math that drives formulary decisions. A brand-name drug might cost $300 per dose. The generic version? $12. That’s not a small difference when you’re managing thousands of patients a year. But it’s not just about the sticker price. Hospitals look at the total cost of care. A cheaper generic that leads to fewer readmissions or shorter hospital stays saves even more. For example, Johns Hopkins switched to a formulary-preferred generic anticoagulant and saved $1.2 million annually without a single increase in adverse events. That’s the kind of result that gets noticed.How Do They Decide Which Generic to Pick?
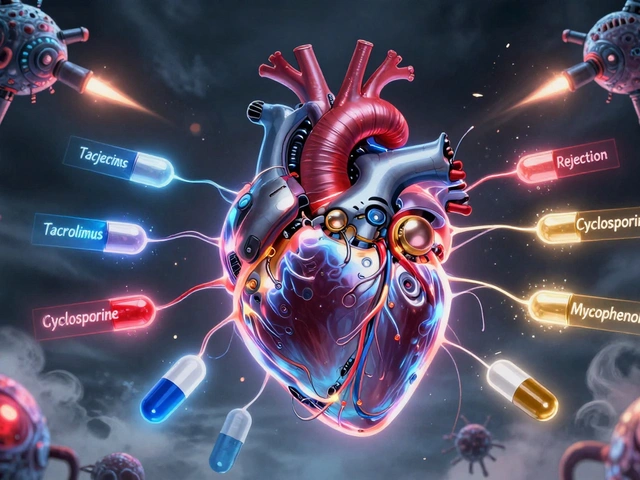
Not all generics are created equal-even if they’re labeled as bioequivalent. The FDA requires generics to be within 80-125% of the brand drug’s absorption rate, but hospitals dig deeper. Here’s how they evaluate:- Therapeutic equivalence: First, they check the FDA’s Orange Book. If a generic is rated AB1, it’s considered interchangeable with the brand.
- Clinical evidence: They review at least 15-20 peer-reviewed studies on efficacy and safety. A drug might be cheap, but if it causes more nausea or dizziness, it gets rejected.
- Adverse event data: Hospitals pull data from the FDA’s Adverse Event Reporting System. If a particular generic manufacturer has a spike in reports of low blood pressure or liver enzyme changes, they take notice.
- Formulation differences: A pill might be the same chemically, but if it’s harder to swallow, dissolves slower, or comes in a different color that confuses elderly patients, it can affect compliance. Pharmacists track this closely.
- Supply chain reliability: In 2022, 268 generic drugs faced shortages. If a manufacturer can’t consistently deliver, the formulary gets pulled-even if the drug is perfect otherwise.

Formulary Tiers and Patient Costs
Most hospital formularies are divided into tiers. Tier 1 is the lowest cost-usually generic drugs with the best evidence and lowest price. Patients pay the least here. Tier 2 might be brand-name drugs with no generic alternative. Tier 3 or 4? Expensive specialty drugs, often requiring prior authorization. This tier system isn’t about pushing patients toward cheaper options. It’s about steering clinicians toward the most effective, safest, and most reliable drugs. When a pharmacist substitutes a generic at the pharmacy counter, they’re following the formulary’s rules-not making a personal choice.Where the System Gets Messy
It sounds clean on paper. But real-world practice? It’s messy. Pharmacists report being stuck between doctors and patients. A physician might want to prescribe a specific generic because “it worked for my last patient.” But if that version has inconsistent bioavailability or a history of supply issues, the formulary committee may have already removed it. That leads to friction. In one survey, 57% of pharmacists said they’ve had arguments with physicians over substitution. Nurses see the fallout too. When a formulary switches from one generic to another, they have to retrain staff. One nurse on AllNurses.com described a case where a new generic antihypertensive looked different and came in a new bottle. Three patients got the wrong dose because staff assumed it was the old version. That’s why many hospitals now require mandatory training every time a formulary change happens. And then there’s the influence of pharmaceutical reps. Even with strict conflict-of-interest rules, some reps still drop off samples, host dinners, or push data that favors their product. A 2021 study in JAMA Internal Medicine found that detailing-sales visits by drug reps-still affects formulary decisions, even in top academic hospitals.
What’s Changing Now?
The rules are evolving. In 2023, the American Society of Health-System Pharmacists (ASHP) and the American Managed Care Pharmacy (AMCP) updated their guidelines to emphasize two big shifts:- Total cost of care: Hospitals no longer just look at the price per pill. They model how a drug affects readmissions, ER visits, and length of stay. A slightly more expensive generic that cuts hospital stays by a day? That’s a win.
- Real-world evidence: Instead of relying only on clinical trials, hospitals now use data from electronic health records. If 10,000 patients on a certain generic had fewer complications, that counts as proof.
Who Benefits?
The system isn’t perfect, but it works. Patients get safer, more consistent care. Hospitals save millions. Insurance systems stay solvent. And when done right, the formulary doesn’t limit care-it protects it. Take hypertension, for example. Over 90% of ACE inhibitor prescriptions in hospitals are generic. Why? Because multiple generics have proven equally effective, and the savings are massive. A patient gets a $5 pill instead of a $150 one. No drop in outcomes. No increase in side effects. Just better value. The real challenge comes with newer drugs-like biosimilars for autoimmune diseases. These aren’t simple generics. They’re complex biologics. Only 37% of hospitals have formal protocols to evaluate them. That gap is growing as more biosimilars enter the market.What’s Next?
By 2028, the Agency for Healthcare Research and Quality predicts all Medicare-certified facilities will be required to have a formal formulary system. That’s not a threat-it’s a recognition that medication decisions can’t be left to chance. The future of hospital formularies is data-driven, transparent, and patient-centered. It’s about using science, not sales pitches, to pick the right drug. And in a world where healthcare costs keep climbing, that’s not just smart-it’s essential.Are generic drugs as safe as brand-name drugs in hospitals?
Yes. All generic drugs approved by the FDA must meet the same strict standards for safety, strength, quality, and performance as brand-name drugs. Hospitals go further-they require evidence from multiple clinical studies and monitor real-world adverse event reports. If a generic shows higher rates of side effects or inconsistent absorption, it’s removed from the formulary.
Why do some doctors resist using generic drugs?
Some doctors worry that generics might be less effective or cause different side effects, especially if they’ve had a bad experience with a specific manufacturer. Others feel they lose control over treatment choices. But research shows that when formularies are based on solid evidence, outcomes don’t suffer. The resistance often comes from outdated beliefs or lack of exposure to high-quality data.
How often do hospital formularies change?
Most academic hospitals review their formularies quarterly. Community hospitals do it twice a year. But urgent changes-like drug shortages or safety alerts-can trigger a review within days. A drug can be added, removed, or restricted at any time based on new data.
Can patients request a non-formulary drug?
Yes, but it’s not automatic. The prescribing doctor must submit a prior authorization request explaining why the non-formulary drug is necessary-often because the patient had an allergic reaction or failed all formulary alternatives. The P&T committee then reviews it. Approval rates vary, but most requests are denied unless there’s strong clinical justification.
Do formularies affect patient outcomes?
When designed properly, they improve outcomes. Hospitals with strong formulary systems see lower rates of medication errors, fewer drug interactions, and reduced hospital readmissions. A 2023 study found that hospitals following ASHP guidelines had 18-22% lower drug costs without any increase in adverse events-meaning better care, not worse.
What’s the difference between a hospital formulary and a Medicare Part D formulary?
Hospital formularies focus on clinical safety and total cost of care within the hospital setting. They’re managed by a committee of clinicians. Medicare Part D formularies are designed for outpatient prescriptions and prioritize patient cost-sharing-using tiered copays to steer patients toward cheaper drugs. Hospital formularies don’t care what the patient pays; they care about what works best in the clinical environment.



Christina Bischof
December 16, 2025 AT 19:45Been on the receiving end of formulary swaps a few times. One time I got a generic that made me dizzy for a week. Turned out it was a different manufacturer. No one told me. Just assumed it was the same. Hospitals need to track manufacturer changes like they track drug interactions.
Lisa Davies
December 17, 2025 AT 06:25Love that hospitals are finally using real-world data 🙌 No more guessing based on old studies. If 10k people took it and didn't die, that counts! 🥳
Nupur Vimal
December 18, 2025 AT 08:00Cassie Henriques
December 19, 2025 AT 11:35Therapeutic equivalence via Orange Book AB1 ratings is table stakes. The real differentiator is pharmacokinetic variance in bioequivalence studies-especially Cmax and AUC0-t confidence intervals. When a generic shows 118% Cmax vs 82% in another, that’s not just ‘similar,’ it’s clinically significant. Add in excipient variability and you’ve got a recipe for non-adherence in polypharmacy patients.
Jake Sinatra
December 20, 2025 AT 21:31This is exactly how healthcare should work. Evidence-based, cost-conscious, and clinically rigorous. Too bad it’s still the exception, not the rule. We need more systems like this, not fewer.
RONALD Randolph
December 22, 2025 AT 18:36YOU THINK YOU’RE SMART, HUH? YOU THINK YOU CAN SAVE MONEY BY SWITCHING PILLS?! WELL, I’VE SEEN PATIENTS DYE THEIR SKIN BLUE FROM A GENERIC ANTIBIOTIC-AND YOU WANT TO TALK ABOUT ‘EVIDENCE’?! THE FDA IS A CORRUPT FACILITY! WE NEED BRANDS-OR WE’LL ALL DIE IN HOSPITALS BECAUSE OF CHEAP CHINA PILLS!!!
Michelle M
December 23, 2025 AT 03:42It’s funny how we treat medicine like a spreadsheet. We optimize for cost, efficiency, and data-but forget that a pill isn’t just a molecule. It’s a promise. A promise that someone will feel better. Sometimes, the quietest victories aren’t in the numbers-they’re in the patient who didn’t have to explain why their medicine looked different this time.
Melissa Taylor
December 24, 2025 AT 08:29So glad to see formularies moving toward pharmacogenomics. My cousin has CYP2D6 poor metabolizer status-she was almost given a drug that would’ve put her in the ICU. If hospitals had tested her first, it would’ve been avoided. This isn’t futuristic-it’s necessary.
John Brown
December 24, 2025 AT 18:19My dad’s on a blood thinner. Switched generics twice last year. The new one made him nauseous. Took three weeks to get the old one back. The pharmacy said ‘it’s the same.’ But it wasn’t. The bottle was different, the pill was smaller, the coating tasted weird. We’re not robots. We notice these things.
Sai Nguyen
December 25, 2025 AT 14:16Benjamin Glover
December 26, 2025 AT 18:58How quaint. A ‘formulary’-as if medicine were a corporate procurement spreadsheet. In the UK, we don’t need committees to decide what’s ‘safe.’ We have NICE. And they don’t care about your ‘real-world evidence’ if the cost-per-QALY isn’t below £20,000. Your system is chaotic. Ours is efficient.
Raj Kumar
December 28, 2025 AT 04:32Yea i read this and its crazy how much work goes into picking a pill. But like... if it works and costs less, why fight it? My uncle got switched to a generic and his bp is better now. Maybe its not perfect but its better than before. Also pharma reps are sketchy, no cap.